Jezper - Fotolia.com
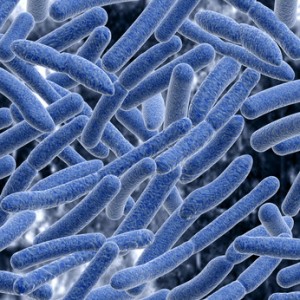
Bacteria is bad. Right?
That is now being rethought. The New York Times has a fascinating article about new research into the “good bacteria” that live in or on the human body — all 100 trillion of them.
They’re needed for digesting food, forming barricades against the bad bacteria, even synthesizing some vitamins. But we’ve known remarkably little about them — what they look like in healthy people, and how they vary amongst individuals.
The Human Microbiome Project has been looking into this, and what they’ve found is pretty cool.
Each person’s collection of microbes, the microbiome, was significantly different from another person’s.
Their work has helped establish criteria for a healthy microbiome, so more is known about how to fix one that isn’t functioning correctly. It also helps figure out what antibiotics do to a microbiome, and how long it takes for the microbiome to recover from antibiotics.
The various microbiomes also help explain why different people react differently to various drugs, and why some people are more vulnerable to certain infectious diseases. When microbiomes cease to function correctly they are thought to contribute to chronic diseases and conditions such as asthma, irritable bowel syndrome, and maybe even obesity.
Dr. David Relman, a Stanford microbiologist, describes the microbiome as analogous to coral, with humans taking the coral role and the bacteria as the many life-forms that live within it. Dr. Barnett Kramer, from the National Cancer Institute in Maryland, says that instead we should instead consider ourselves mostly made of microbes. “We may just serve as packaging.”
The microbiome starts to grow at birth, said Lita Proctor, program director for the Human Microbiome Project. As babies pass through the birth canal, they pick up bacteria from the mother’s vaginal microbiome.
“Babies are microbe magnets,” Dr. Proctor said. Over the next two to three years, the babies’ microbiomes mature and grow while their immune systems develop in concert, learning not to attack the bacteria, recognizing them as friendly.
Babies born by Caesarean section, Dr. Proctor added, start out with different microbiomes, but it is not yet known whether their microbiomes remain different after they mature. In adults, the body carries two to five pounds of bacteria, even though these cells are minuscule — one-tenth to one-hundredth the size of a human cell. The gut, in particular, is stuffed with them.
“The gut is not jam-packed with food; it is jam-packed with microbes,” Dr. Proctor said. “Half of your stool is not leftover food. It is microbial biomass.” But bacteria multiply so quickly that they replenish their numbers as fast as they are excreted.
The bacteria also help the immune system, Dr. Huttenhower said. The best example is in the vagina, where they secrete chemicals that can kill other bacteria and make the environment slightly acidic, which is unappealing to other microbes.
Including the microbiome as part of an individual is, some researchers said, a new way to look at human beings.
It was a daunting task, though, to investigate the normal human microbiome. Previous studies of human microbiomes had been small and had looked mostly at fecal bacteria or bacteria in saliva in healthy people, or had examined things like fecal bacteria in individuals with certain diseases, like inflammatory bowel disease, in which bacteria are thought to play a role.
But, said Barbara B. Methé, an investigator for the microbiome study and a microbiologist at the J. Craig Venter Institute, it was hard to know what to make of those studies.
“We were stepping back and saying, ‘We don’t really have a population study. What does a normal microbiome look like?’ ” she said.
The first problem was finding completely healthy people for the study. The investigators recruited 600 subjects, ages 18 to 40, poking and prodding them. They brought in dentists to probe their gums, looking for gum disease, and pick at their teeth, looking for cavities. They brought in gynecologists to examine the women to see if they had yeast infections. They examined skin and tonsils and nasal cavities. They made sure the subjects were not too fat and not too thin. Even though those who volunteered thought they filled the bill, half were rejected because they were not completely healthy. And 80 percent of those who were eventually accepted first had to have gum disease or cavities treated by a dentist.
When they had their subjects — 242 men and women deemed free of disease in the nose, skin, mouth, gastrointestinal tract and, for the women, vagina — the investigators collected stool samples and saliva, and scraped the subjects’ gums and teeth and nostrils and their palates and tonsils and throats. They took samples from the crook of the elbow and the folds of the ear. In all, women were sampled in 18 places, including three sites in the vagina, and men in 15. The investigators resampled subjects three times during the course of the study to see if the bacterial composition of their bodies was stable, generating 11,174 samples.
To catalog the body’s bacteria, researchers searched for DNA with a specific gene, 16S rRNA, that is a marker for bacteria and whose slight sequence variations can reveal different bacterial species. They sequenced the bacterial DNA to find the unique genes in the microbiome. They ended up with a deluge of data, much too much to study with any one computer, Dr. Huttenhower said, creating “a huge computational challenge.”
The next step, he said, is to better understand how the microbiome affects health and disease and to try to improve health by deliberately altering the microbiome.
But, Dr. Relman said, “we are scratching at the surface now.”
It is, he said, “humbling.”